Why Diabetics May Face Issues With Acidity Regulation In Their Bodies.
It starts with the activity of the carbonic anhydrase enzyme.
One of the common blood tests that diabetics undertake regularly is to measure the levels of HbA1c in their blood. Our bodies require the haemoglobin protein to transport oxygen through our blood to the various cells in the body.
The problem that diabetics face is that they have too much glucose in their blood. Glucose can react with haemoglobin proteins to form the HbA1c protein, which is otherwise known as glycated haemoglobin:
The Humble Aldehyde Is Something That We Ought To Be Very Wary Of When Consuming Processed Foods.
It’s quite interesting to note these days what we can eat and what we shouldn’t be eating. Even if the food product is actually edible… the metabolites may not be regarded as safe. We know a few things about what not to consume in overly large quantities. Sugar, we know, isn’t that great. Alcohol, we know that we shouldn’t be drinking too much of. Polyunsaturated fats (or even partially hydrogenated fats) aren’t that great either.
The idea being that this HbA1c sugar-protein conjugate isn’t as great at moving molecular oxygen through the body. When the haemoglobin protein has been glycated, it cannot be counted upon to transport oxygen to the cells and tissues in our body as effectively as normal haemoglobin.
This poor oxygen transport can ultimately lead to limb amputations:
Why Diabetics Are Likely To Face Future Issues With Limb Amputations.
Apparently, maggot debridement therapy is a mode of treatment for diabetic patients with foot injuries. According to this article: In maggot debridement therapy, sterile maggots are used to clean up a wound as the maggots are able to break down dead tissue and speed up the healing process.
It is a fallacious assumption to think that diabetes is just a case of having too much glucose in the blood — because these glucose molecules are chemically reactive and can potentially react with any biomolecules or cells within our body.
We have to understand that the hydrochloric acid being produced for digesting foods in our stomach is also based on enzymatic activity.
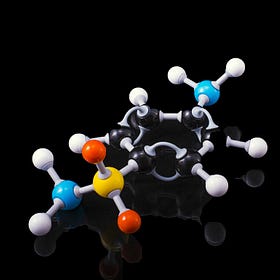
The acids in the stomach are produced based on the activity of the carbonic anhydrase (CA) enzyme. CA is an enzyme “that assists rapid inter-conversion of carbon dioxide and water into carbonic acid, protons and bicarbonate ions”.
In our digestive system, CA is responsible for the production of gastric acid by the parietal cells.
Similarly, CA in the kidneys is thought to maintain the acid/base equilibrium in our blood based on controlling bicarbonate resorption from our urine before excretion, with the mechanism outlined here.
In our kidneys and our stomach, the CA enzyme is extremely important for maintaining the appropriate levels of acidity, which would have a significant bearing on our digestive functions otherwise.
So the problem that a diabetic would face, therefore, would be related to the potential glycation of the CA enzymes in the stomach and in the kidneys, because CA is a protein as haemoglobin is. If haemoglobin can be glycated and lose its functionality in one’s body, it wouldn’t be surprising to see that CA can be affected in the same way via glycation.
If the CA enzyme is damaged via glycation, it cannot do its work in maintaining stomach acidity or blood/urine pH control. These symptoms would manifest themselves in a reduced food digestion ability or blood acidosis over time. They’re just symptoms of excess glucose in the blood.
And that’s just the CA enzyme undergoing structural changes as a result of reactions with glucose. What happens if there were going to be structural changes to proteins in the brain?
Protein misfolding (structural changes) will definitely impact how the brain functions. Would that be why some people consider Alzheimer’s to be Type 3 diabetes?
But the issue here is that the excessive sugar in our blood is reactive and can cause issues with the proteins and enzymes that are necessary for carrying out various reactions within our body. If these reactions are not running optimally, we can see our bodies become more sluggish over time.
The more enzymes that are damaged, the more suboptimally we’d be operating in our daily lives. But yet it isn’t something that is of concern to us - until the symptoms become irreversibly damaging, no>
For the readers out there who know people living through chronic diabetes: how informed are these diabetic patients about what diabetes can do to their digestive systems in the long run?
Do feel free to share this article and hit the “subscribe” button to get more updates about the science concepts in nutrition and health, all deconstructed nicely for your convenient perusal!