The Oddities Behind Wound Healing In Our Bodies
Before new life is created, there must be more death and destruction first.
In this physical world filled with a ton of atrocious human clumsiness, just about anything is possible. We don’t have to look very far to find prizes such as the Darwin awards to celebrate human stupidity:
They recognize individuals who have supposedly contributed to human evolution by selecting themselves out of the gene pool by dying or becoming sterilized via their own actions.
I know most of us here aren’t like that.
But we can be clumsy and unfortunate at times to do things that affect ourselves — I do stub my toe or knock my head against a low ceiling sometimes. I’ve also managed to fracture six bones in one foot while attempting a LeBron James-esque chase-down block in my younger years.
But whatever the case is, injuries aren’t fun. They’re going to cause death and destruction to various individual cells and tissues in our body.
When we experience that injury, we first have to clear out all that dead cells and tissues (or cell debris), which would otherwise impede the synthesis of new cells.
It’s like doing a home renovation - we have to clear out everything inside a home before we can actually do modifications to its interior.
We know when we’re injured, for sure, especially when we do something that ends up injuring ourselves.
The feeling of pain or the loss of function in the limb? For example, when we experience a sprain or a fracture in our foot, we aren’t going to be able to walk normally until the injury has been healed.
When we do suffer that injury, there will be damage to the cells and surrounding tissues within that region.
The pain that we experience is a symptom of an acute inflammation response from the immune system at the site of the injury, where the production of pro-inflammatory cytokines is ramped up significantly:
Redness and heat are due to increased blood flow to the inflamed area; swelling is due to accumulation of fluid; pain is due to release of chemicals that stimulate nerve endings; and loss of function is due to a combination of factors. These signs are manifested when acute inflammation occurs on the surface of the body, but not all of them will be apparent in acute inflammation of internal organs.
The acute inflammation recruits macrophages to the injury site — the inflammation response is localized to where the injury is. If I have a sprain on my left foot, I’m not going to feel the pain on my right foot — but my left foot will feel terribly sore.
Inflammation — Like It Or Not, It’s Here To Stay.
It would suffice to say that the word “inflammation” is causing quite a stir these days. When we’re injured, for instance, the site of injury is experiencing acute inflammation, and that contributes to unpleasant sensations of pain and swelling that we can feel
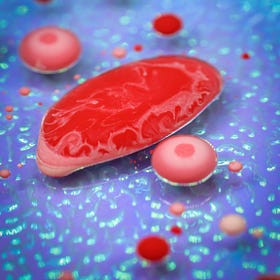
Under this pro-inflammatory environment, the macrophages that dominate the overall macrophage population are known as the M1 phenotype. These guys are the main fighters that protect the wound from bacterial infections and clear out all the debris and dead cells. When the tissue begins to repair, we’d see a shift in the dominant macrophage population to be of the M2 phenotype:
Initially, pro-inflammatory macrophages, traditionally referred to as “M1” macrophages, infiltrate after injury in order to clean the wound of bacteria, foreign debris and dead cells. In acute wounds, as the tissue begins to repair, the overall macrophage population transitions to one that promotes anti-inflammatory effects (traditionally and collectively referred to as “M2” macrophages), and the migration and proliferation of fibroblasts, keratinocytes and endothelial cells to restore the dermis, epidermis and vasculature, respectively. This process will eventually close the wound and produce a scar.
If I were to tear a muscle, the M1 macrophages have to start clearing out all the frayed ends of the torn muscle before the M2 macrophages can start working on closing up the wound.
The Importance Of The Macrophage In The Immune System
The macrophage is one of those immune cells in our body that does quite a fair bit of things without us thinking about it. We’re exposed to so many microbes and virues in the environment on a daily basis, and some of them can penetrate through the skin and mucosal barriers that act as the first line of defence to those foreign invaders:
They work in tandem based on the prevailing intensity of the inflammation response. We’ve got the pro-inflammatory cytokines and the anti-inflammatory cytokines that are in a tug-of-war with each other and the various types of cells that can produce those different cytokines. This tug-of-war is a crucial factor in determining how quickly our wounds are going to heal.
So, of course, when we suffer an injury, the body isn’t going to start repairing itself right away.
There is a sequential process involved.
The surviving (but frayed) pieces of biological material must first be killed off via apoptosis and then be digested and eliminated — the M1 macrophages are key for doing all of that in a highly pro-inflammatory environment. These M1s also produce matrix metalloproteinase (MMP) enzymes that aid in the destruction of biological material and the non-biological support scaffolds in the body that we term as the extracellular matrix (ECM).
These are the very same MMP enzymes that can work on digesting atherosclerotic plaques.
Now, Seriously, What's So Tricky About Cholesterol?
This article is the final part of a 3 part miniseries. The first 2 parts can be found at:
We need the MMPs to destroy all that before we can commence repairs.
It’s like how land developers have to bulldoze and destroy old buildings completely to build new ones on the sites where the old buildings once stood.
Would we see a speedier or slower recovery if the pro-inflammatory response were to prevail longer than necessary?
Slower, of course.
While we always wish the most painless and speediest recoveries for our friends and family who have experienced some form of physical injury, we have to be mindful that there must be destroyed before the actual repairs can commence, and how quickly the body can deal with the destruction phase is also important.
But where there is destruction and inflammation, there will always be pain and discomfort.
As such, the road to recovery may still be pretty uncomfortable — my fractured foot was so sore on the first few nights that it was almost impossible even to sleep properly. Surgery was necessary for fixing the bones back into their proper positions, too.
In severe diabetics, for instance, the glycation of the hemoglobin proteins in their blood results in a reduced oxygen transport rate throughout the body.
As such, when they injure their feet, they’re going to take an extremely long time to recover — and some may actually require amputation from gangrenous complications because the macrophages cannot handle the workload of eliminating dead tissue and defending against bacterial invasions with a reduced oxygen supply going to the foot.
Why Diabetics Are Likely To Face Future Issues With Limb Amputations.
Apparently, maggot debridement therapy is a mode of treatment for diabetic patients with foot injuries. According to this article:
That leaves the diabetic’s foot stuck in the rut of the M1 phase without getting to the M2 phase.
The chronically elevated inflammation that triggers insulin resistance in Type 2 diabetics isn’t of any help, either. It’s not going to support the transition into the M2 phase that readily, for sure.
And if a pro-inflammatory environment does support the M1 macrophages in producing more MMPs, what will happen with our hearts and our joints because MMPs are also employed in coercing a plaque to rupture or for the destruction of joint cartilage?
Perhaps that’s why older people find it more difficult to recover from an injury, especially if they’ve gone through major surgeries.
Because aging also does disrupt the inflammatory balance in the body.
The Biochemistry Behind The Aging Process
Aging is unfortunately an inevitable problem that all of us humans will face. Multiple aspects of our lives can be affected as we age.
Perhaps that’s why we call it inflammaging.
Do feel free to share this article and hit the “subscribe” button to get more updates about the science concepts in nutrition and health, all deconstructed nicely for your convenient perusal!