The Same Enzyme Family That Destroys Joints Can Contribute To Heart Attacks.
Here's how it does so.
Heart disease, as we know it, is and has been responsible for the deaths of many people on this planet. The data presented by the World Health Organisation indicate that:
The world’s biggest killer is ischaemic heart disease, responsible for 16% of the world’s total deaths. Since 2000, the largest increase in deaths has been for this disease, rising by more than 2 million to 8.9 million deaths in 2019. Stroke and chronic obstructive pulmonary disease are the 2nd and 3rd leading causes of death, responsible for approximately 11% and 6% of total deaths respectively.
And we can see that the second killer behind heart disease is that of stroke.
Those two issues are linked together, unfortunately.
The problem being that we can’t pinpoint high cholesterol as the sole reason for heart disease, however:
Understanding How Cholesterol Accumulates In Our Body
The whole problem with health and healthcare these days is that things can get so complicated such that we have no idea how to make any head or tail out of it.
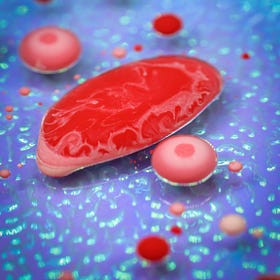
We can see how it accumulates in our body, and then that triggers off a biochemical response that gets our immune cells involved.
Because the cholesterol firstly gets eaten up by live macrophage cells, which will eventually end up being entrapped within a plaque.
The Importance Of The Macrophage In The Immune System
The macrophage is one of those immune cells in our body that does quite a fair bit of things without us thinking about it. We’re exposed to so many microbes and virues in the environment on a daily basis, and some of them can penetrate through the skin and mucosal barriers that act as the first line of defence to those foreign invaders:
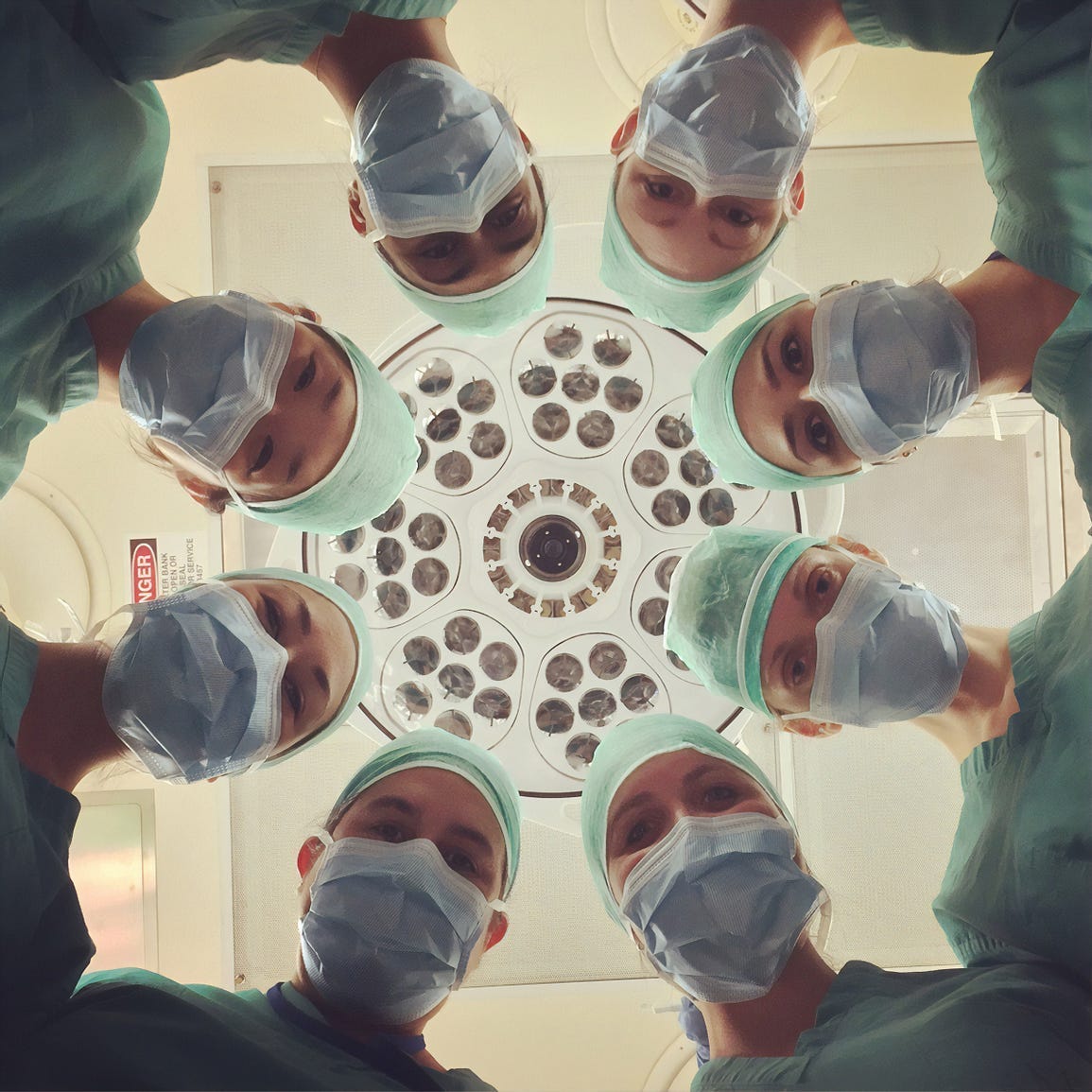
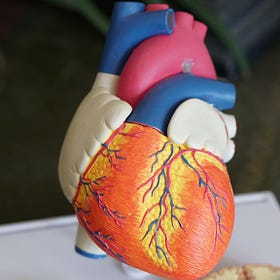
What we do need to understand is that an atherosclerotic plaque in an artery is sealed off by a layer of collagen. The macrophages that are entrapped in the plaque would find living conditions highly untenable. Some of them would die within the plaque, creating a necrotic and highly pro-inflammatory environment. This pro-inflammatory environment is very conducive for stimulating the surviving macrophages to produce (matrix metalloproteinase) MMP enzymes, which can digest away the collagen cap that is sealing off the atherosclerotic plaque.
Which means that these MMPs can also digest away the collagen found in joint cartilage in the development of osteoarthritis — all these MMPs are being produced at the command of an inflammatory signal:
Inflammation — Like It Or Not, It’s Here To Stay.
It would suffice to say that the word “inflammation” is causing quite a stir these days. When we’re injured, for instance, the site of injury is experiencing acute inflammation, and that contributes to unpleasant sensations of pain and swelling that we can feel until the injury has been healed. Ditto, when we do catch a bout of the flu as well.
When we injure any of our joints, a localised pro-inflammatory signal is sent out from the site of injury. This signal brings about with it pain and swelling, and also indicates that macrophages are being recruited over to the site of damage.
The MMPs produced by these macrophages will digest away the damaged sections of collagen, such that a new collagen structure can be synthesised in place. Hence, the joint is unable to function normally at the onset of the injury and may not be able to bear full weight until the new collagen structure has been synthesised.
However, if we do injure the same joint repeatedly, such as it is in the case of athletes who put much more strain on their bodies while training as compared to other people on the street, there is a higher possibility that we will develop osteoarthritis along the way too. Athletes who rush their recovery process are also at risk of more frequent re-injuries, especially when they do not allow their bodies adequate time to completely heal.
In the case of mild chronic inflammation, we know that the entrapped macrophages and the free macrophages (swimming about in the blood) do have a higher tendency to produce more MMPs — the prevailing inflammation signals in the body will tell them to produce more.
Which will potentially result in an acute symptom of a heart attack if the collagen cap on an atherosclerotic plaque were to be digested and weakened to the point of the plaque rupturing.
Now, Seriously, What's So Tricky About Cholesterol?
This article is the final part of a 3 part miniseries. The first 2 parts can be found at:
It’s because the macrophages in the blood (and those entrapped in the atherosclerotic plaques) are producing MMPs in pro-inflammatory environments to digest away the plaque.
If the plaque will rupture and its contents leak out into the blood, the clotting factors in our blood will cause those plaque contents to form a clot. If the clot were to block the flow of blood in a majory artery leading to the heart, we would see the development of a heart attack forming.
However, because a person experiencing heart disease is already experiencing chronic inflammation, the macrophages in their blood would also be producing more MMPs.
These MMPs would be able to digest away collagen structures in other parts of the body, which can bring about visible signs of aging such as the premature collapse of skin structures to form skin wrinkles.
As our joints are also made out of collagen, joint pain can also occur:
What Pain In The Joints Indicates For The Rest Of Our Body.
Osteoarthritis is a common issue that plagues most people who experience chronically painful joints that have lost a fraction of their original functions. We feel it as we age and as our bodies degenerate.
We can therefore see that the biochemical mechanism that triggers plaque rupture is the same biochemical mechanism that eliminates damaged joint cartilage.
It does seem to be such a rhetorical question, however: “If you do have heart disease, how bad is your joint pain?”
Because those two problems are linked.
Do feel free to check out 10 Nutrients That Support A Healthy Heart to see how our diet can influence our heart health!
10 Nutrients That Support A Healthy Heart
Supporting cardiovascular health is not an easy thing to do. We eat food. We exercise. We get stressed by work. We sleep. All these actions do contribute to the overall state of our immune system.
Also, do feel free to share this article and hit the “subscribe” button to get more updates about the science concepts in nutrition and health, all deconstructed nicely for your convenient perusal!








Always fascinating content! Thank you!