Why Diabetics Are Likely To Face Future Issues With Limb Amputations.
We'd have to look at all those downstream effects to understand more.
Apparently, maggot debridement therapy is a mode of treatment for diabetic patients with foot injuries. According to this article:
In maggot debridement therapy, sterile maggots are used to clean up a wound as the maggots are able to break down dead tissue and speed up the healing process.
For people with diabetes, foot ulcers are a common risk — and one that often leads to infection, hospitalisation, or in worst case scenarios, amputation.
If we were to go one level up in terms of thinking, we’d be asking:
Why is it that a diabetic patient cannot eliminate all that dead tissue as effectively as they ought to be doing?
The answer, of course, lies in the ability of the body to perform autophagy.
Much like any supermarket requires a cleanup crew to clear up accidental spills and messes before things start to go rotten and nasty, the body also has an autophagy mechanism to clear up dead cells.
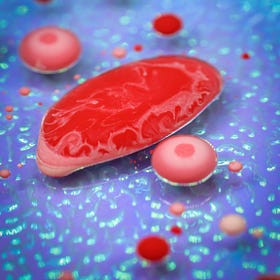
Basically, we have phagocyte cells such as our immune system’s macrophages, which engulf and decompose all the dead cells into something simpler to build up new cells.
Unfortunately, it is said in this article that “dysfunction of autophagy is associated with obesity and type 2 diabetes”.
Meaning that a diabetic body’s ability to conduct autophagy is severely compromised.
And that’s also a concern with the ability of their immune systems to function efficiently.
The issue right here is that our cells all need certain nutrients to survive and function. One of these nutrients is, of course, oxygen.
Every cell uses oxygen as an electron acceptor during the energy generation process, which results in molecular oxygen being reduced down to water.
For a macrophage to conduct its phagocyte activities, it needs to generate energy first — and an oxygen supply is necessary for it to function properly.
For that oxygen supply to be consistent, we’d need to have it bind to haemoglobin (Hb) proteins in our blood, such that it can then be carried through the blood to feed the cells in our body.
Now, the problem in a diabetic body is that they have higher levels of glycated haemoglobin proteins (HbA1c) in their blood, which will ultimately affect the binding capability of oxygen.
The difference between Hb and HbA1c is that HbA1c has a binding affinity for oxygen that is TEN TIMES more than normal Hb.
In other words, HbA1c is more selfish than Hb- it refuses to let go of the oxygen that is bound to it, much like how some kids have to be coaxed more just to share their toys and games (I was once upon a time like that myself, so I can’t point fingers at anyone!).
The problem now is that a diabetic has higher levels of HbA1c in their blood. As the oxygenated Hb proteins get pumped out of the blood, the organs nearest to the heart will extract oxygen from the normal Hb proteins. The HbA1c proteins get pumped down to the legs, where it is more difficult for the cells at our feet to extract oxygen from the HbA1c proteins.
I’m sure many of you would have noticed that it’s never good living downstream of a river — the downstream inhabitants are basically at the mercy of the upstream inhabitants.
Take the Mekong River in Southeast Asia, for instance. Its source is in China, where the Chinese government brilliantly built eleven dams on the river.
The damming resulted in a damning effect on the downstream nations of Thailand, Laos, Vietnam, and Cambodia. Because all the nutrient-rich sediments and water volume was held back by those dams, the ecosystems and food production systems in the downstream countries were affected significantly — more so when the region experienced a drought.
In the same way, when our blood is going to be transporting less AVAILABLE oxygen, the cells furthest downstream will be the most affected.
By the time the blood reaches the feet, the feet would be looking at an insufficient blood supply.
I’m not saying that it’s completely insufficient for a normal day. However, when there is increased oxygen demand, such as it is in the case of an injury where macrophages need extra oxygen to carry out their repair work, would the macrophages be lacking oxygen or not have enough to do what they’re supposed to be doing effectively enough?
We’d be forced to admit that the oxygen supply would be insufficient. As a result, the macrophage activity in clearing out the dead tissue gets worsened in a diabetic, wouldn’t it?
Unfortunately, as the macrophages are required for wound healing as well as defensive activity against foreign invaders, we’d see that a diabetic’s foot wound would take longer to heal, and while it is taking longer to heal, it would also be more prone to infections, because the oxygen supply is so darned bad.
Hence parameters such as the VO2max are good to know. VO2max is a parameter used to quantify the maximum oxygen consumption rates that our bodies can achieve while exercising.
(V stands for volumetric rate, O2 is oxygen, and max is maximum.)
It is, of course, a measure of one’s physical fitness. Diabetics, of course, are prone to lower VO2max consumption rates than their healthy counterparts. Because one of the factors for diabetes development is exercise, or rather, a lack thereof.
So it does make sense that a person who has diabetes most probably lacks the exercise frequency and intensity, therefore having a lower VO2max, therefore when not exercising, will experience even lower levels of oxygen transport because all that HbA1c ain’t conducive for transporting oxygen through the blood.
And therefore, their autophagy functions get dysregulated.
And therefore, when they get open cuts to their feet, the risk of gangrene development and amputation increases.
Because when necrosis sets in on a dead cell, the situation’s going to turn nasty. Much like an uncleared mess of tomato ketchup in Aisle 3 of a supermarket. Any uncleared ketchup is going to turn putrid and smell bad. (As an Uber driver, I did not appreciate passengers throwing up in my backseat after a night out at the pub either.)
Much like what happens in necrosis.
Necrotic cells will release more pro-inflammatory cytokines, and the subsequent infection/inflammation to a necrotic wound can potentially give rise to a toxic shock.
The Importance Of The Macrophage In The Immune System
The macrophage is one of those immune cells in our body that does quite a fair bit of things without us thinking about it. We’re exposed to so many microbes and virues in the environment on a daily basis, and some of them can penetrate through the skin and mucosal barriers that act as the first line of defence to those foreign invaders:
We Live In A World Drugged Out On Sugar, And We’re Silently Paying The Price For It.
We face an endless barrage of sugar at every turn. The doughnuts in that picture look great, don’t they? What about the sugar in ice cream? Other cakes and pastries? Chocolate bars? Fruits? Cereals? Juices and soft drinks? Wherever we go, we are bombarded by it, much like how scantily dressed women are seen in many different advertisements today.
Inflammation — Like It Or Not, It’s Here To Stay.
It would suffice to say that the word “inflammation” is causing quite a stir these days. When we’re injured, for instance, the site of injury is experiencing acute inflammation, and that contributes to unpleasant sensations of pain and swelling that we can feel
The least that a diabetic would experience would be more post-activity soreness and a slower recovery rate, which of course, points right back at a dysfunctional immune system again!
Do feel free to share this article and hit the “subscribe” button to get more updates about the economics and science concepts in nutrition and health, all deconstructed nicely for your convenient perusal!